The Essential Guide to Diabetic Foot Health in Arizona
In the Valley of the Sun, staying active is a way of life. But for the millions of Arizonans living with diabetes, a simple foot problem can quickly threaten that lifestyle and independence. Diabetes is now the leading cause of non-traumatic lower limb amputations in the United States. While this sounds frightening, the majority of these amputations are preventable with regular podiatry check ups.
Your feet are often the first place that complications of diabetes show up. Understanding how and why these complications happen, and knowing how to get ahead of them, can be the difference between staying active and facing serious health setbacks. This is why establishing a trusted relationship with your podiatrist at Red Mountain Footcare is one of the most important steps in protecting your health and your future.
The Dual Threat: How Diabetes Directly Affects Your Feet
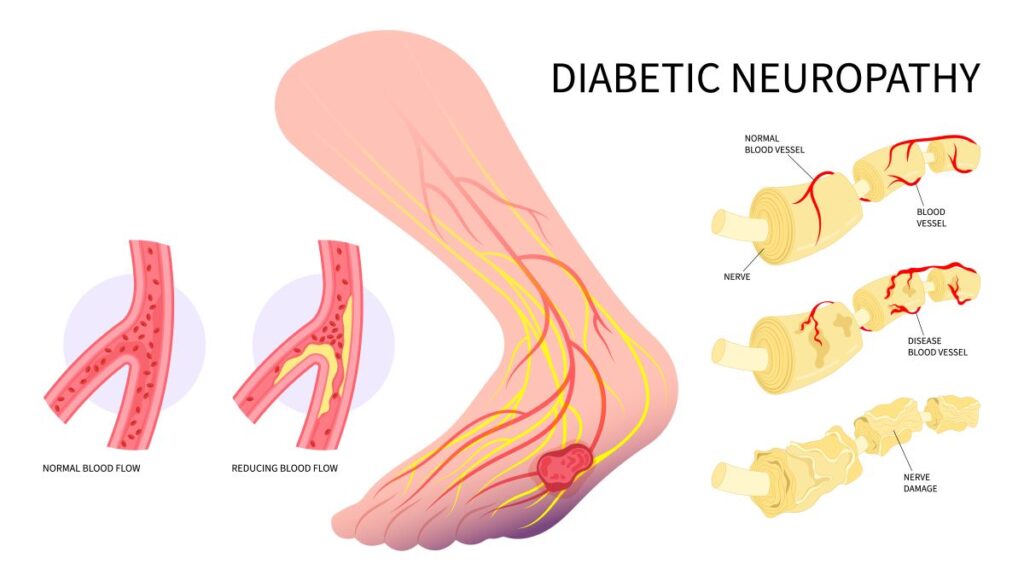
If you have diabetes, your feet are more vulnerable than you might think. Two common complications of diabetes combine to create the “perfect storm” for foot problems: diabetic neuropathy and peripheral arterial disease.
What is Diabetic Neuropathy? Understanding Nerve Damage
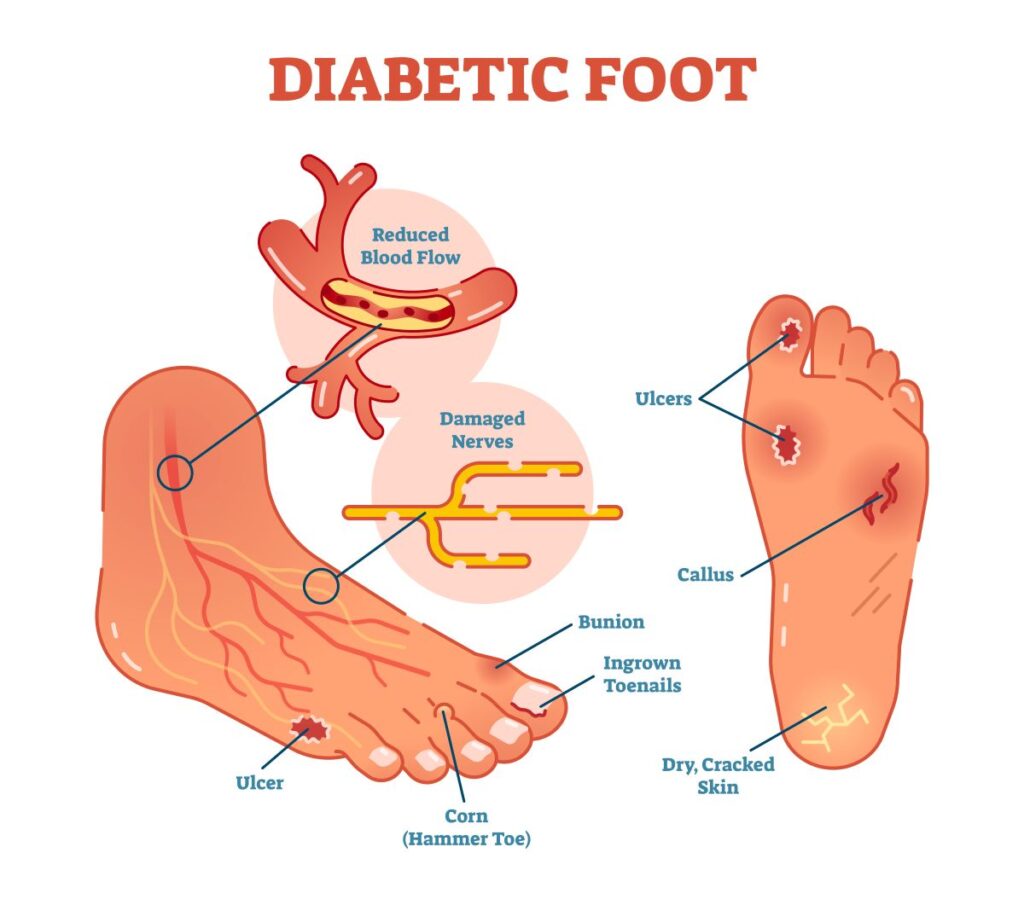
Diabetic Neuropathy is nerve damage from high blood sugar that affects the body’s extremities: hands, feet, legs, and arms. High blood sugar levels over time can damage nerve fibers throughout your body, but the legs and feet are most often affected. Diabetic neuropathy typically leads to numbness, tingling, burning, or a total loss of feeling in the feet.
Common Foot Health Concerns with Diabetic Neuropathy
What makes this dangerous is that you might not notice small injuries like a blister from a new pair of shoes, a cut from trimming your toenails, or even a pebble stuck in your shoe. Because you cannot feel these injuries, there’s a higher risk of delaying treatment. What starts as a small scratch could develop into an infected gash before you realize something is wrong.
What is Peripheral Arterial Disease (PAD)? What to Know About Poor Circulation
Diabetes also damages your blood vessels, causing them to narrow and reduce blood flow to your feet. This is called peripheral arterial disease, or PAD for short. When your circulation is poor, your body has a harder time delivering the oxygen and nutrients needed for healing.
Even a minor cut or scratch can turn into a non-healing ulcer that becomes infected. This combination of lost sensation and poor healing is why routine diabetic foot care is so crucial.
Unique Feet Risk Factors for Diabetics in Arizona
Living with diabetes anywhere requires vigilance, but Arizona’s unique climate and lifestyle add extra challenges.
Dry, Arid Climate and Cracked Skin
Our famously low humidity is tough on everyone’s skin, but for those with diabetes, it can be particularly dangerous. Dry, cracked skin, especially on the heels, can create fissures that act as open doors for bacteria. A simple crack for others can be a major risk for infection if you have diabetes.
Injuries from Heat and Sun Exposure
Arizona summers get dangerously hot. Whether you live here year-round or just part of the year, you’re probably used to the climate and the safety precautions you need to take. But every now and then, we all have moments where we forget simple heat protection.
If you have neuropathy, you may not feel hot pavement or sun exposure burning your feet. Severe burns can easily blister and become infected, especially on the tops of your feet where skin is thinner. The risks are highest during our extreme summer months, when even a few minutes barefoot outside can cause significant injury.
Active, Outdoor Lifestyles
Arizona is a great place to live for outdoor enthusiasts. Whether you love hiking, walking, camping, or just spending time in the pool, there are many opportunities to get outside and stay active. Unfortunately, rocky trails and uneven ground can create pressure points, blisters, or small cuts that can be dangerous on neuropathic feet.
The Domino Effect: From a Small Sore to a Serious Complication
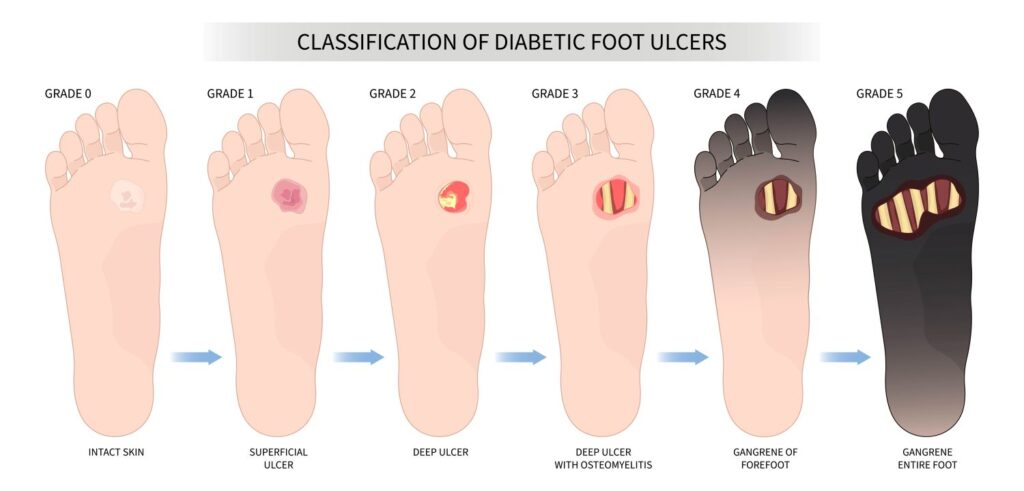
It is important to understand how quickly a minor foot issue can escalate for someone with diabetes. Imagine you develop a small blister from a new pair of shoes. Diabetic neuropathy prevents you from feeling it, then poor circulation from PAD prevents the area from healing well. Within a few days, the wound can become infected.
Dangers of Untreated Injuries
In a worst-case-scenario, the wound stays unnoticed and untreated while the infection spreads to deeper tissues. At this stage, a non-healing diabetic foot ulcer can develop, which, in severe cases, may progress to gangrene. For some patients, amputation may be the only option to prevent life-threatening infection.
All of this is completely preventable with early intervention and proactive, professional care from your podiatrist.
What to Expect During a Diabetic Foot Care Appointment
At Red Mountain Footcare, we know that prevention is the best medicine. Our diabetic foot care plan is designed to catch problems early, manage ongoing risks, and keep you walking confidently. Here is what you can expect from your regular visits with our team:
Comprehensive Visual Inspection
We thoroughly examine your feet for any changes you may have missed, including redness, swelling, sores, or breaks in the skin. Even small signs can indicate deeper problems.
Neurological Assessment
Using specialized tools like a monofilament (a fine, flexible wire), we check for loss of sensation in your feet. This is critical for diagnosing neuropathy and its severity. Identifying loss of feeling early allows for extra protection and education.
Vascular Assessment
We assess pulses and blood flow in your feet. If there is evidence of poor circulation, we can recommend appropriate interventions or work with your primary care team for additional vascular evaluation.
Biomechanical and Gait Analysis
Your foot structure and the way you walk are evaluated to spot pressure points or areas at risk for calluses and ulcers. By identifying these areas, we can help you avoid problems before they start. Your podiatrist might recommend a different shoe style or a custom orthotic to protect your feet.
Professional Nail and Callus Care
Trimming thick, fungal, or ingrown toenails, and safely reducing painful calluses, is best left to professionals in a medical office. Attempting this at home increases the risk of injury and infection. Some patients try to incorporate this care with pedicures at nail salons, but that can also be dangerous for diabetics.
While you might find a nail technician with good intentions, they simply aren’t trained to handle conditions related to diabetes. Additionally, nail salons do not follow the same sanitation protocols as a medical office. Your podiatrist’s tools are sterilized with machines like an autoclave, then individually packaged to prevent cross-contamination.
Top Ways to Maintain Healthy Feet as a Diabetic
Preventing diabetic foot complications is a team effort. Here’s what you can do every day:
- Check Your Feet Regularly for Small Injuries: Make it a daily habit, just like brushing your teeth. Use a mirror to see all areas, especially the bottoms of your feet.
- Wear Proper Footwear: Never walk barefoot, even indoors. Choose well-fitted shoes with good support and moisture-wicking socks to protect against injury and keep feet dry.
- Moisturize Carefully: Use a good moisturizer to prevent dry, cracked skin, but avoid applying it between the toes to prevent fungal growth.
- Follow Your Treatment Plan: If your doctor prescribes treatment, always follow through with their recommendations and keep your entire care team up-to-date. For many diabetics, an endocrinologist or specialized primary care doctor is often the front of line for ongoing health concerns. Medications prescribed at one office should always be discussed when visiting another to prevent interactions.
- Avoid Non-Medical Settings for Foot and Nail Maintenance: Most cosmetologists and nail technicians aren’t trained to handle diabetic footcare, and most nail salons are not allowed to treat anyone with suspected nail fungus.
- Contact Your Doctor for Guidance: If you notice any changes, no matter how small, call your podiatrist immediately.
Prevention and Early Detection: The Power of the Regular Visit
The greatest value in working with Red Mountain Footcare is our ability to catch problems you may not see or feel. Early detection and prompt treatment can make all the difference. Each visit, we tailor advice to your unique needs, recommending the best footwear, self-inspection routines, and moisturizing strategies suited for the Arizona climate. Our goal is to help you live well and stay active.
Why Choose Arizona Red Mountain Footcare?
For patients dealing with serious complications, our team is uniquely equipped to help. Dr. Spencer Hardy, DPM, is a Lower Extremity Nerve Specialist and Wound Care Specialist. He is registered with several local hospitals, which ensures continuity of care if an injury, wound, or condition cannot be treated in office.